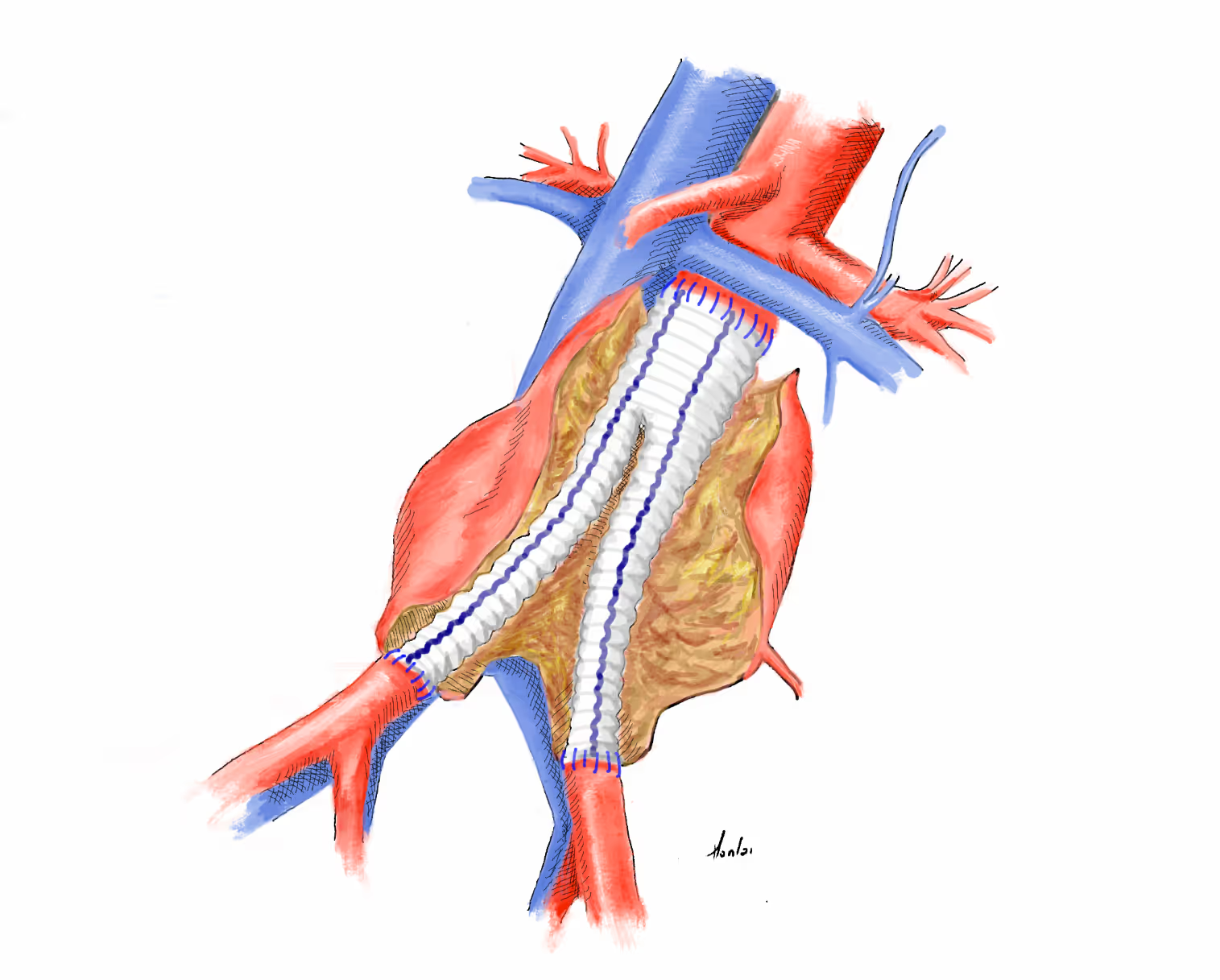
An abdominal aortic aneurysm bifurcated graft interposition is a surgical procedure where a prosthetic graft is used to replace a weakened or enlarged section of the abdominal aorta. The graft is bifurcated, allowing it to connect to the iliac arteries, thereby restoring normal blood flow and preventing the aneurysm from rupturing. If the ischemia time is expected to last more than 2 hours, we start with a distal (iliac) anastomosis
Educational objectives
.avif)
The Vascular International (VI) School for Vascular Surgery is dedicated to advancing the training and education of vascular surgical techniques through the use of lifelike models. With patient safety as the top priority, VI continuously strives to enhance vascular surgery training, ensuring the highest standards of safe and effective open and endovascular patient care.
About Us